
TREAT THE FIELD WITH PHOTODYNAMIC THERAPY (PDT)
Field therapies address both clinically
visible and subclinical lesions1,2
Subclinical actinic keratosis (AK) lesions are often found in the deeper layers of the epidermis surrounding visible AKs.1,2
Areas surrounding visible AK lesions can harbor the same genetic changes as the AK lesions themselves.2
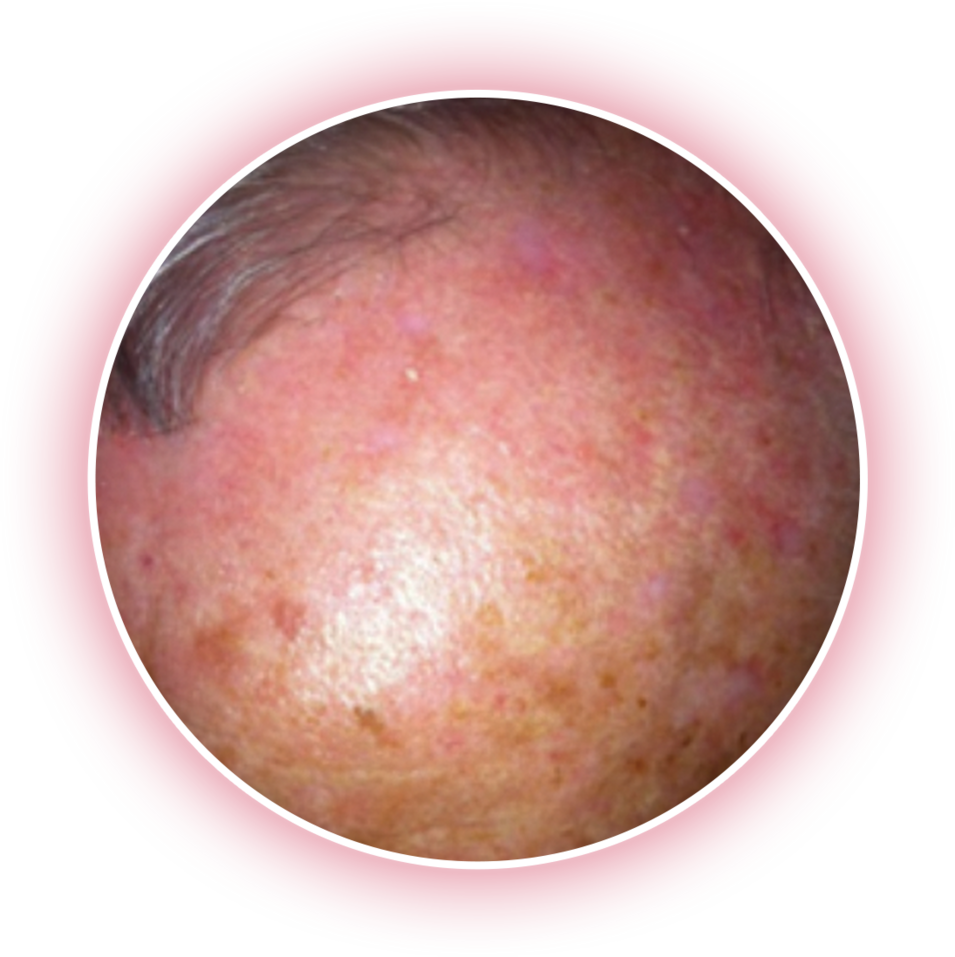
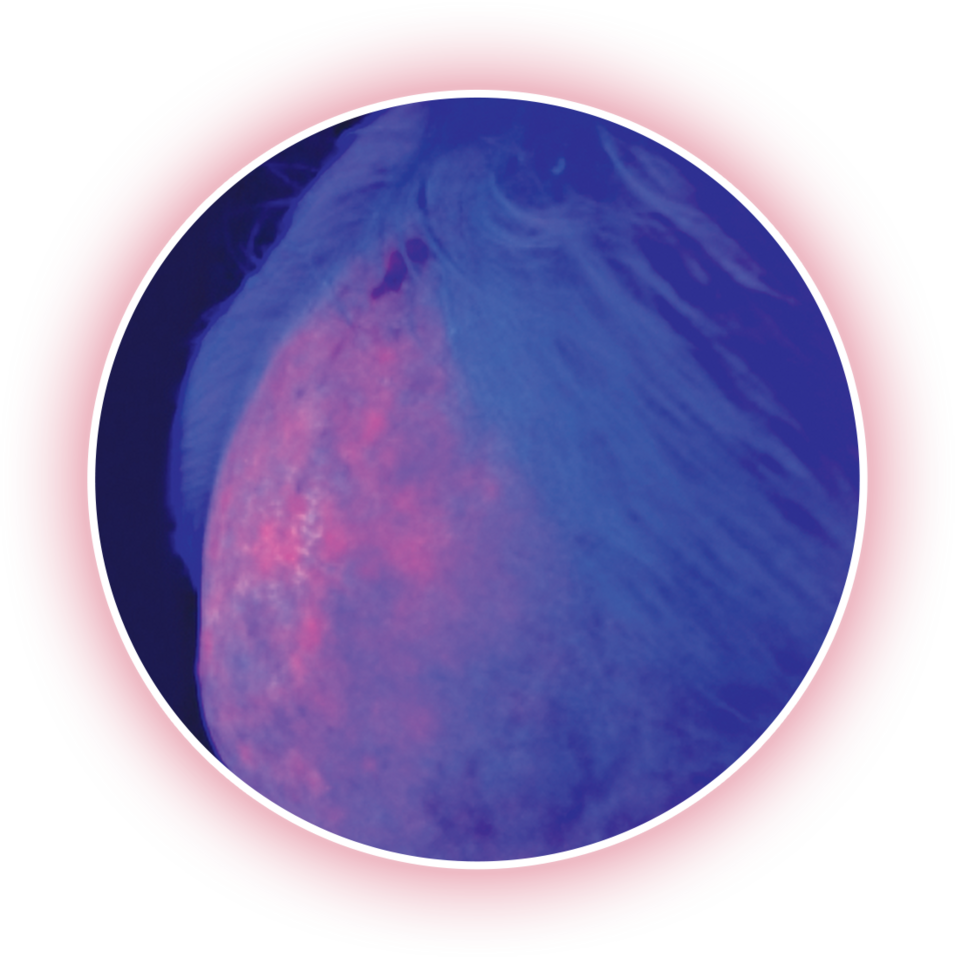
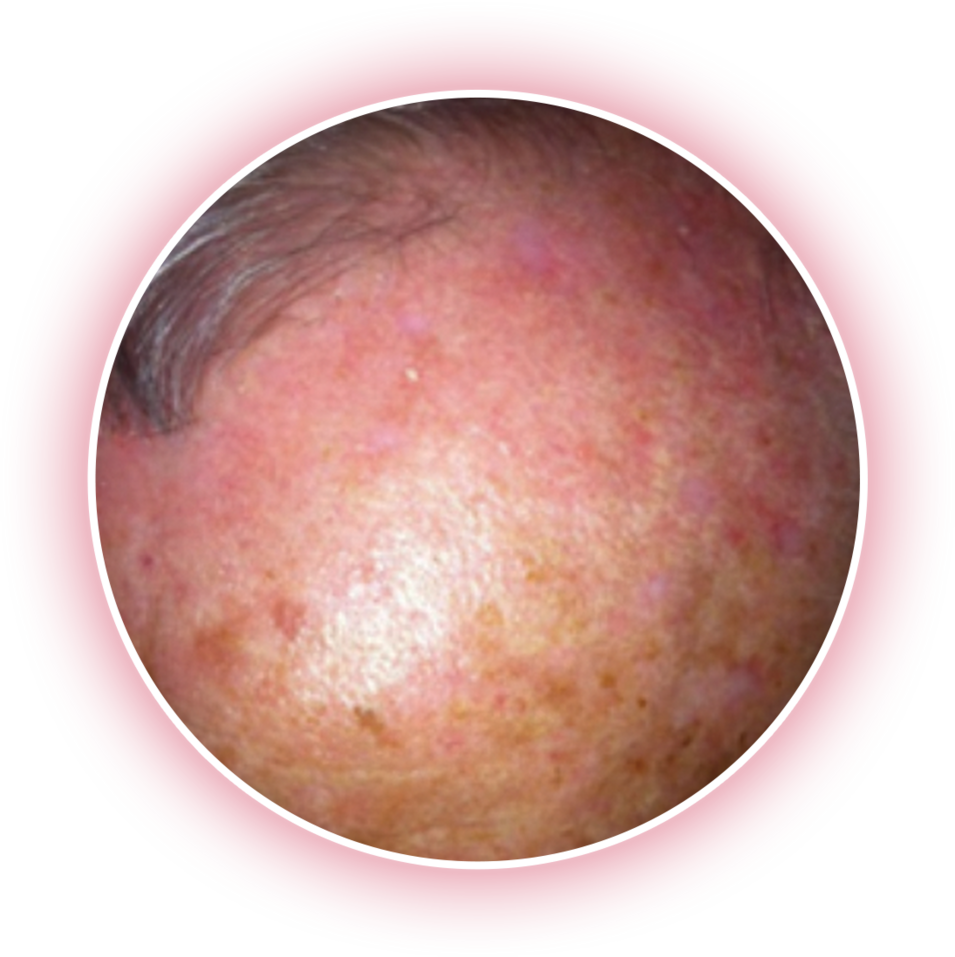
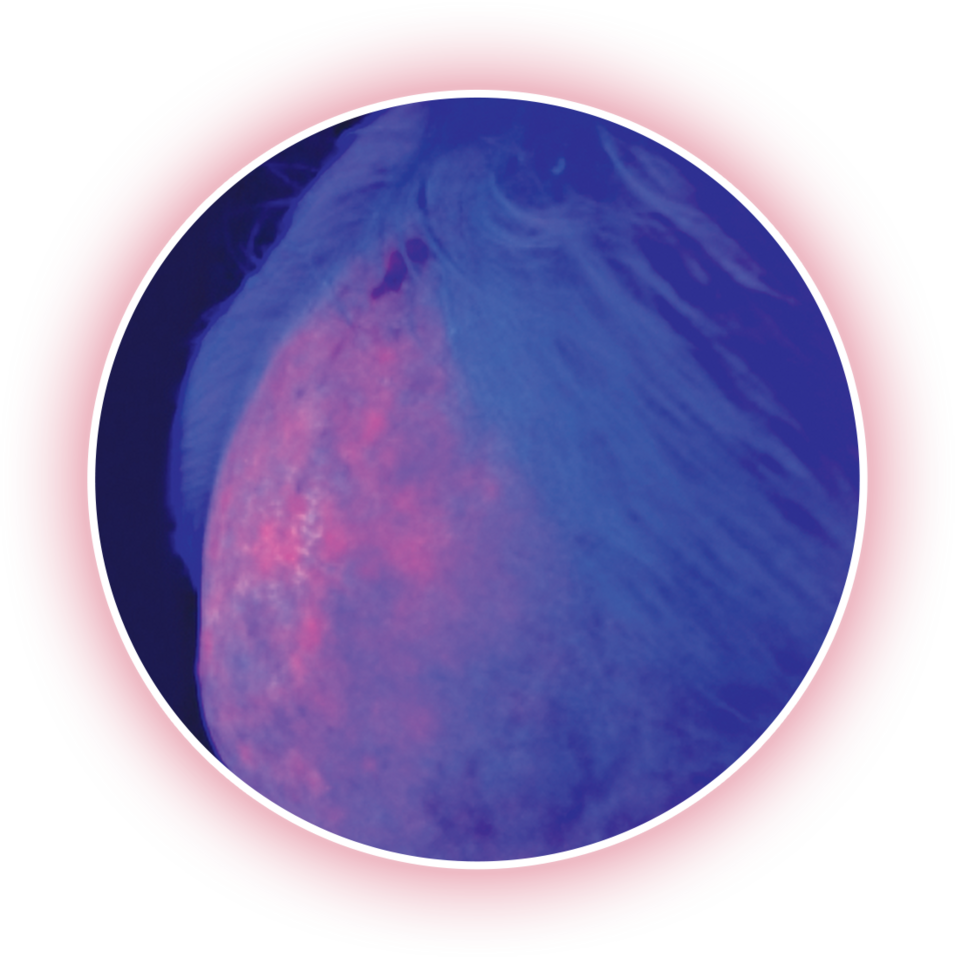
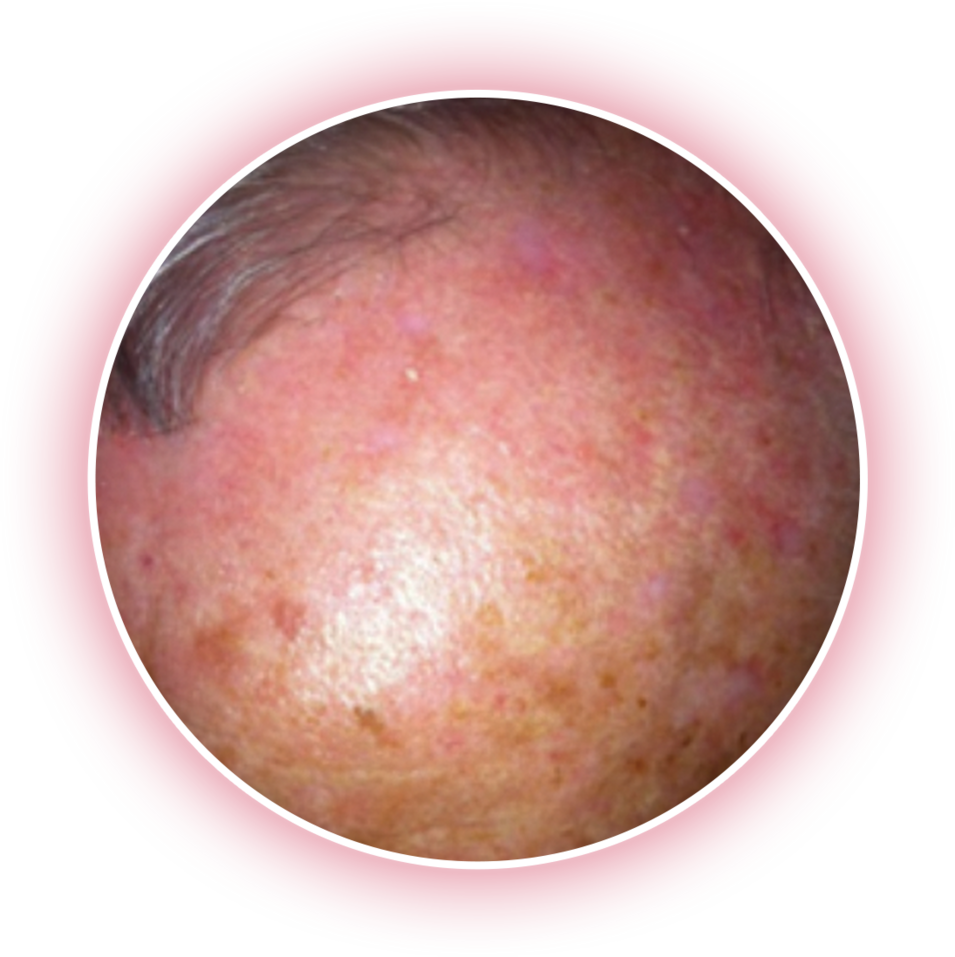
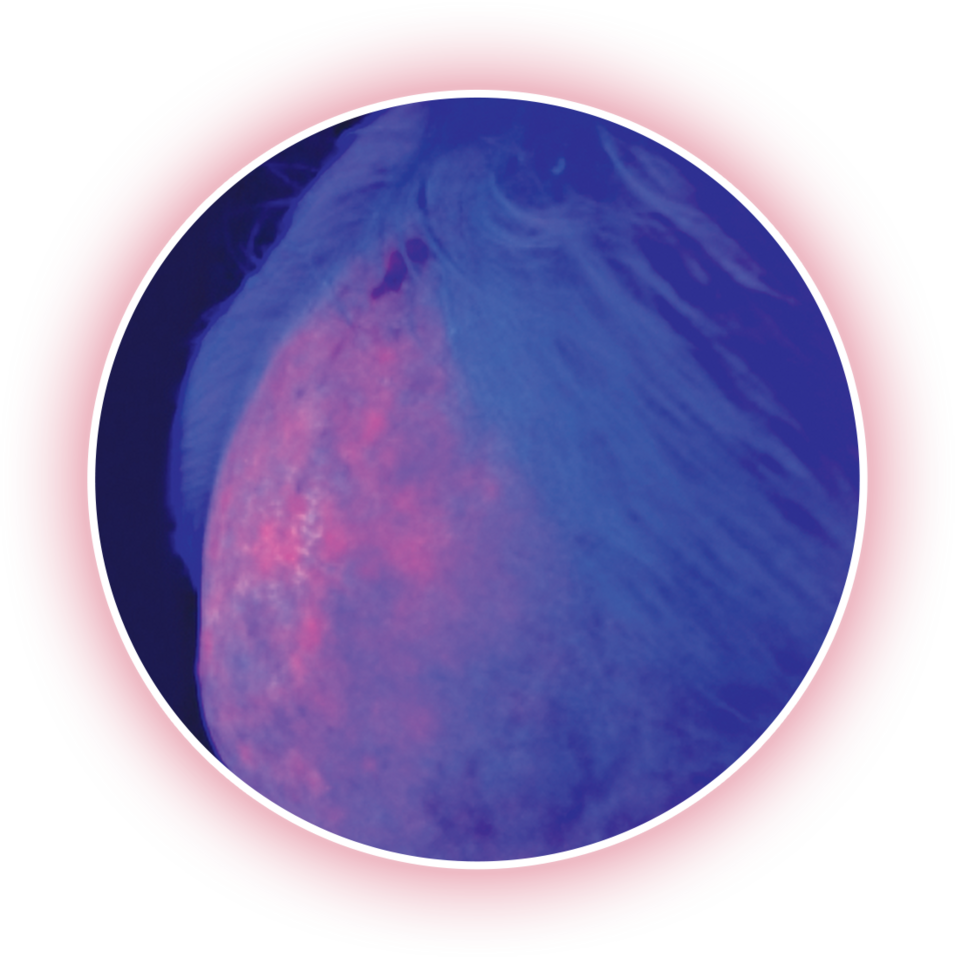
Fluorescence imaging reveals underlying lesions.
Red fluorescent areas visualized under black light after a 3-hour incubation with aminolevulinic acid HCl topical gel, 10%.
PDT offers a field-directed yet targeted approach
to help treat visible and subclinical AK lesions3,4

Allowing you to manage AK in affected areas of the face and scalp4,5
May help prevent the clinical appearance of new lesions4,6
PDT helps you maintain control
over your patient’s condition3,5
Short treatment times—less than a day
A maximum of 2 treatment visits
Patient-applied topical therapies present adherence challenges
Adherence to patient-applied topical therapies declines as the duration of therapy increases. In one study:

of patients were non-adherent with 3-4 weeklong treatments7

of patients were non-adherent with 4-8 weeklong treatments7

of patients were non-adherent with 6-12 weeklong treatments7
These data were derived from an observational, non-interventional, prospective study including 305 patients. Patients were required to fill in a questionnaire after treatment with topical drugs indicated for AK over several weeks.
Discover the advantages of using AMELUZ® (aminolevulinic acid HCl) topical gel, 10% for PDT
Schedule a PDT consult to review
field-directed treatment options


TREAT THE FIELD WITH PHOTODYNAMIC THERAPY (PDT)
Field therapies address both clinically
visible and subclinical lesions1,2
Subclinical actinic keratosis (AK) lesions are often found in the deeper layers of the epidermis surrounding visible AKs.1,2
Areas surrounding visible AK lesions can harbor the same genetic changes as the AK lesions themselves.2
Fluorescence imaging reveals underlying lesions.
Red fluorescent areas visualized under black light after a 3-hour incubation with aminolevulinic acid HCl topical gel, 10%.
PDT offers a field-directed yet targeted approach
to help treat visible and subclinical AK lesions3,4

Allowing you to manage AK in affected areas of the face and scalp4,5
May help prevent the clinical appearance of new lesions4,6
PDT helps you maintain control
over your patient’s condition3,5
Short treatment times—less than a day
A maximum of 2 treatment visits
Patient-applied topical therapies present adherence challenges
Adherence to patient-applied topical therapies declines as the duration of therapy increases. In one study:

of patients were non-adherent with 3-4 weeklong treatments7

of patients were non-adherent with 4-8 weeklong treatments7

of patients were non-adherent with 6-12 weeklong treatments7
These data were derived from an observational, non-interventional, prospective study including 305 patients.
Patients were required to fill in a questionnaire after treatment with topical drugs indicated for AK over several weeks.
Discover the advantages of using AMELUZ® (aminolevulinic acid HCl) topical gel, 10% for PDT
Schedule a PDT consult to review field-directed treatment options


TREAT THE FIELD WITH
PHOTODYNAMIC THERAPY (PDT)
Field therapies address both
clinically visible and
subclinical lesions1,2
Subclinical actinic keratosis (AK) lesions are often found in the deeper layers of the epidermis surrounding visible AKs.1,2
Areas surrounding visible AK lesions can harbor the same genetic changes as the AK lesions themselves.2
Fluorescence imaging reveals underlying lesions.
Red fluorescent areas visualized under black light after a 3-hour incubation with aminolevulinic acid HCl topical gel, 10%.
PDT offers a field-directed yet targeted approach
to help treat visible and subclinical AK lesions3,4

Allowing you to manage AK in affected areas of the face and scalp4,5
May help prevent the clinical appearance of new lesions4,6
PDT helps you maintain
control over your
patient’s condition3,5
Short treatment times — less than a day
A maximum of 2 treatment visits
Patient-applied topical therapies present adherence challenges
Adherence to patient-applied topical therapies declines as the duration of therapy increases. In one study:

of patients were non-adherent with 3-4 weeklong treatments7

of patients were non-adherent with 4-8 weeklong treatments7

of patients were non-adherent with 6-12 weeklong treatments7
These data were derived from an observational, non-interventional, prospective study including 305 patients.
Patients were required to fill in a questionnaire after treatment with topical drugs indicated for AK over several weeks.
Discover the advantages of using AMELUZ® (aminolevulinic acid HCl) topical gel, 10% for PDT
Schedule a PDT consult to review field-directed treatment options

INDICATION AND IMPORTANT SAFETY INFORMATION
INDICATION
AMELUZ® (aminolevulinic acid hydrochloride) topical gel, 10%, a porphyrin precursor, in combination with photodynamic therapy using BF‑RhodoLED® lamp, is indicated for the lesion-directed and field-directed treatment of actinic keratoses of mild-to-moderate severity on the face and scalp.
IMPORTANT SAFETY INFORMATION
AMELUZ® (aminolevulinic acid hydrochloride) topical gel, 10% with BF‑RhodoLED® lamp
AMELUZ®, containing 10% aminolevulinic acid hydrochloride, is a non-sterile gel formulation for topical use only. Not for ophthalmic, oral, or intravaginal use.
AMELUZ®, in conjunction with lesion preparation, is only to be administered by a health care provider. Photodynamic therapy with AMELUZ® involves preparation of lesions, application of the product, occlusion and illumination with BF‑RhodoLED®. The application area should not exceed 20 cm2 and no more than 2 grams of AMELUZ® (one tube) should be used at one time. Lesions that have not completely resolved shall be retreated 3 months after the initial treatment. Refer to BF‑RhodoLED® user manual for detailed lamp safety and operating instructions. Both patient and medical personnel conducting the PDT should adhere to all safety instructions.
AMELUZ® shall not be used by persons who have known hypersensitivity to porphyrins or any of the components of AMELUZ®, which includes soybean phosphatidylcholine. AMELUZ® should also not be used for patients who have porphyria or photodermatoses.
Hypersensitivity reactions have been reported with the use of AMELUZ® prior to photodynamic therapy (PDT). AMELUZ® should be washed off and appropriate therapy instituted. Inform patients and their caregivers that AMELUZ may cause hypersensitivity, potentially including severe courses (anaphylaxis).
Transient Amnestic Episodes have been reported during postmarketing use of AMELUZ® in combination with photodynamic therapy (PDT). If patients experience amnesia or confusion, discontinue treatment. Advise them to contact the healthcare provider if the patient develops amnesia after treatment.
Eye exposure to the red light of the BF‑RhodoLED® lamp during PDT must be prevented by protective eyewear. Direct staring into the light source must be avoided. AMELUZ® increases photosensitivity. Patients should avoid sunlight, prolonged or intense light (e.g., tanning beds, sun lamps) on lesions and surrounding skin treated with AMELUZ® for approximately 48 hours following treatment whether exposed to illumination or not.
AMELUZ® has not been tested on patients with inherited or acquired coagulation disorders. Special care should be taken to avoid bleeding during lesion preparation in such patients. Any bleeding must be stopped before application of the gel. AMELUZ® should not be used on mucous membranes or in the eyes.
Local skin reactions at the application site were observed in about 99.5% of subjects treated with AMELUZ® and narrow spectrum lamps. The very common adverse reactions (≥10%) during and after PDT were application site erythema, pain/burning, irritation, edema, pruritus, exfoliation, scab, induration, and vesicles. Most adverse reactions occurred during illumination or shortly afterwards, were generally of mild or moderate intensity, and lasted for 1 to 4 days in most cases; in some cases, however, they persisted for 1 to 2 weeks or even longer. Severe pain/burning occurred in up to 30% of treatments.
There have been no formal studies of the interaction of AMELUZ® with other drugs. Concomitant use of the following photosensitizing medications may increase the phototoxic reactions after PDT: St. John’s wort, griseofulvin, thiazide diuretics, sulfonylureas, phenothiazines, sulphonamides, quinolones, and tetracyclines.
There are no available data on AMELUZ® use in pregnant women to inform a drug associated risk. No data are available regarding the presence of aminolevulinic acid in human milk, the effects of aminolevulinic acid on the breastfed infant or on milk production. Safety and effectiveness in pediatric patients below the age of 18 have not been established as AK is not a condition generally seen in the pediatric population. No overall differences in safety or effectiveness were observed between elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Please read the US Full Prescribing Information for AMELUZ® and/or US User Manual of BF‑RhodoLED® lamp available together at https://www.ameluz.com/PI.
You are encouraged to report side effects of AMELUZ®. Please contact Biofrontera Inc. at 1‑844‑829‑7434 or FDA at 1‑800‑332‑1088 or www.fda.gov/medwatch.
References: 1. Berman B, Amini S, Valins W, Block S. Pharmacotherapy of actinic keratosis. Expert Opin Pharmacother. 2009;10(18):3015-3031. 2. Stockfleth E. The importance of treating the field in actinic keratosis. J Eur Acad Dermatol Venereol. 2017;31(Suppl 2):8-11. 3. Reinhold U. A review of BF-200 ALA for the photodynamic treatment of mild-to-moderate actinic keratosis. Future Oncol. 2017;13(27):2413-2428. 4. de Berker D, McGregor JM, Mohd Mustapa MF, Exton LS, Hughes BR. British Association of Dermatologists’ guidelines for the care of patients with actinic keratosis 2017. Br J Dermatol. 2017;176(1):20-43. 5. AMELUZ [prescribing information]. Woburn, MA: Biofrontera Inc; 2021. 6. Reinhold U, Dirschka T, Ostendorf R, et al. A randomized, double-blind, phase III, multicentre study to evaluate the safety and efficacy of BF-200 ALA (Ameluz) vs. placebo in the field-directed treatment of mild-to-moderate actinic keratosis with photodynamic therapy (PDT) when using the BF‑RhodoLED lamp. Br J Dermatol. 2016;175(4):696-705. 7. Shergill B, Zokaie S, Carr A. Non-adherence to topical treatments for actinic keratosis. Patient Prefer Adherence. 2014;8:35-41.